What is Ankylosing Spondylitis?
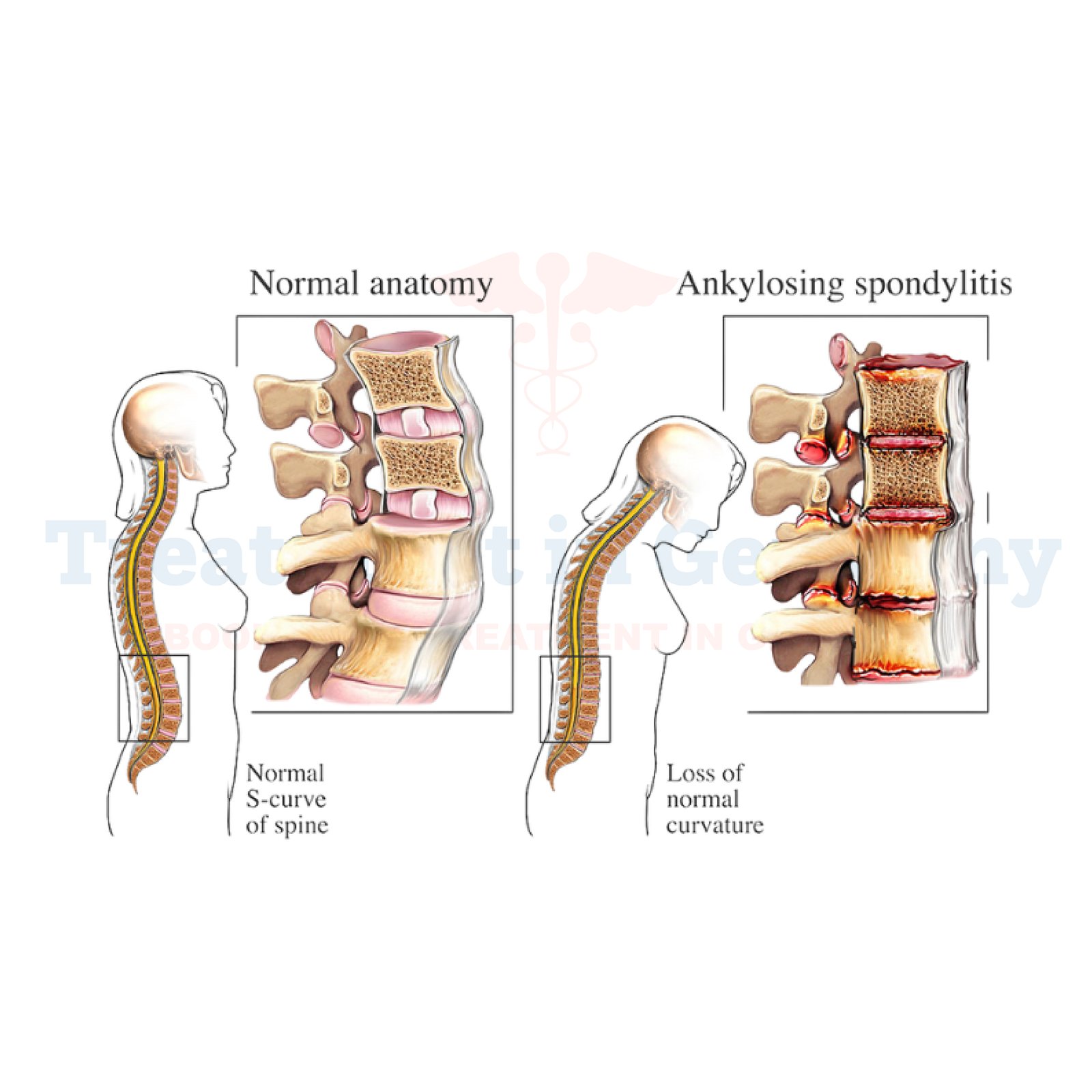
Ankylosing Spondylitis (AS) is a chronic inflammatory condition that primarily affects the spine, causing stiffness, pain, and potentially leading to the fusion of spinal vertebrae over time.
It belongs to a group of disorders known as spondyloarthropathies, which involve inflammation of the joints and ligaments.
Side Effects of Ankylosing Spondylitis
The symptoms of Ankylosing Spondylitis extend beyond the spine, impacting other joints such as hips, shoulders, and knees.
Patients may experience fatigue, reduced flexibility, and in severe cases, breathing difficulties due to restricted chest expansion. Additionally, inflammation can affect organs such as the eyes (uveitis) and the bowel (inflammatory bowel disease).
How is Ankylosing Spondylitis Diagnosed?
Diagnosing Ankylosing Spondylitis involves a combination of medical history, physical examination, imaging studies like X-rays and MRI scans, and blood tests to detect markers of inflammation such as C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR).
A key diagnostic criterion is the presence of inflammatory back pain lasting more than three months, typically worse in the mornings and improving with exercise.
Potential Treatment of Ankylosing Spondylitis
Treatment aims to alleviate symptoms, slow disease progression, and improve quality of life. In Germany, management often begins with non-steroidal anti-inflammatory drugs (NSAIDs) to reduce pain and inflammation.
Physiotherapy and regular exercise programs tailored to maintain spinal mobility are crucial in managing AS. Biologic medications, such as TNF-alpha inhibitors (e.g., adalimumab, infliximab), are prescribed for patients who do not respond adequately to NSAIDs or develop severe disease.

.webp)
 (1).webp)

.webp)
 (1).webp)


.webp)
 (1).webp)

.webp)
 (1).webp)
