What is Benign Prostatic Hyperplasia (BPH)?
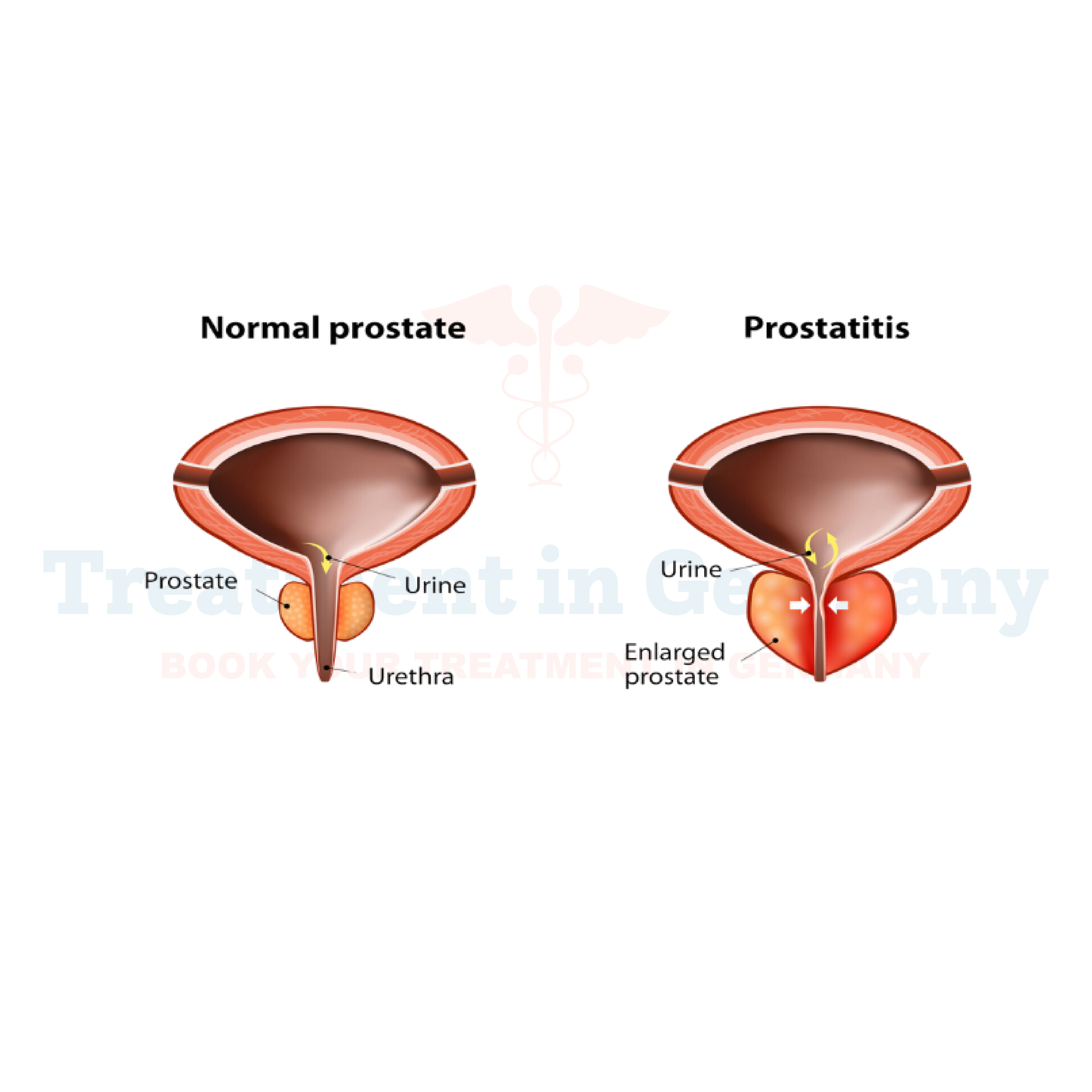
Benign Prostatic Hyperplasia (BPH) is a common condition affecting men as they age. It involves the non-cancerous enlargement of the prostate gland, which is located just below the bladder and surrounds the urethra.
As the prostate enlarges, it can press against the urethra and obstruct the flow of urine, leading to various urinary symptoms. Unlike prostate cancer, BPH does not increase the risk of cancer but can significantly affect your quality of life.
Side Effects of Benign Prostatic Hyperplasia (BPH)
The symptoms of Benign Prostatic Hyperplasia can vary but often include:
- Frequent Urination: Especially at night, known as nocturia.
- Urgency to Urinate: A sudden and strong need to urinate.
- Difficulty Starting Urination: Trouble initiating the urine stream.
- Weak Urine Stream: A noticeable decrease in the strength of the urine flow.
- Incomplete Bladder Emptying: Feeling that the bladder is not fully emptied after urination.
- Straining to Urinate: Having to push or strain to start or maintain the urine flow.
These symptoms can disrupt daily activities and impact overall well-being.
How is Benign Prostatic Hyperplasia (BPH) Diagnosed?
Diagnosis of Benign Prostatic Hyperplasia typically involves several steps:
- Medical History and Symptoms Review: Your doctor will ask about your symptoms and medical history.
- Physical Examination: This usually includes a digital rectal exam (DRE) to assess the size and condition of the prostate.
- Urinary Flow Test: Measures the strength and amount of your urine stream.
- Post-Void Residual Volume Test: Determines how much urine remains in your bladder after urination.
- Prostate-Specific Antigen (PSA) Test: Measures levels of PSA in the blood, which can help rule out prostate cancer.
- Ultrasound or Urodynamic Testing: In some cases, imaging or additional tests may be used to evaluate the prostate and urinary system.
Potential Treatment of Benign Prostatic Hyperplasia (BPH)
Treatment options for Benign Prostatic Hyperplasia vary depending on the severity of your symptoms and their impact on your quality of life. They include:
- Lifestyle Changes: Modifications such as reducing fluid intake before bedtime, avoiding caffeine and alcohol, and regular exercise can help alleviate symptoms.
- Medications: Several types of medications are available, including:
- Alpha Blockers: Relax the muscles in the prostate and bladder neck to improve urine flow.
- Alpha Reductase Inhibitors: Help shrink the prostate by blocking the hormone that causes its growth.
- Combination Therapy: Sometimes, a combination of medications is used for better results.
- Minimally Invasive Procedures: These techniques can help relieve symptoms with less risk and recovery time compared to surgery. Options include:
- Transurethral Microwave Thermotherapy (TUMT): Uses microwave energy to destroy excess prostate tissue.
- Transurethral Needle Ablation (TUNA): Uses radiofrequency energy to destroy prostate tissue.
Surgical Treatments: For more severe cases, surgical options might be necessary, such as:
- Transurethral Resection of the Prostate (TURP): Removes excess prostate tissue through the urethra.
- Laser Surgery: Uses lasers to remove or vaporize prostate tissue.
👉 Contact us for further information and receive a complimentary consultation.

.webp)
 (1).webp)

.webp)
 (1).webp)


.webp)
 (1).webp)

.webp)
 (1).webp)
