What is Cryptorchidism (Undescended Testicle)?
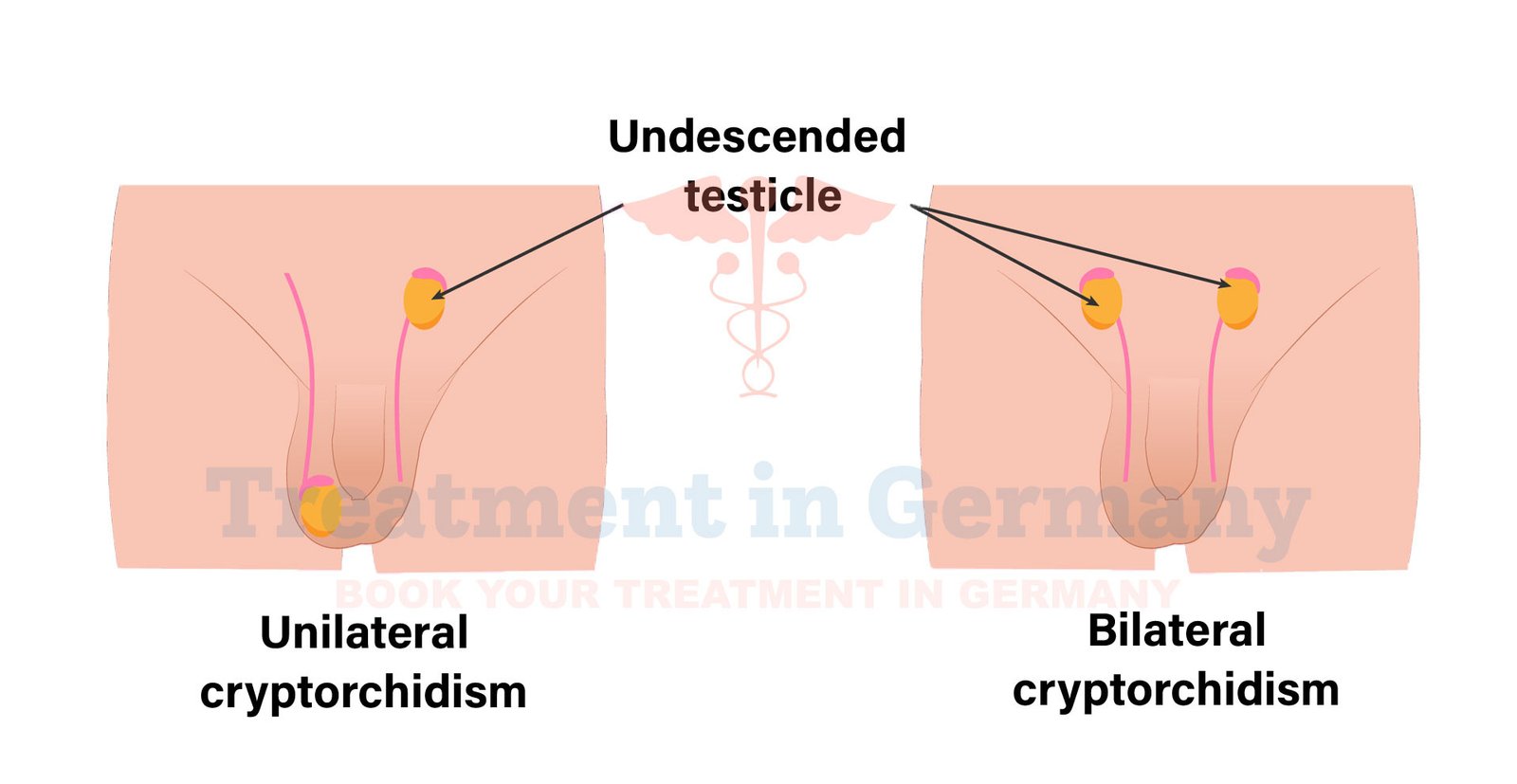
Cryptorchidism, commonly known as an undescended testicle, is a condition where one or both of the testicles fail to descend into the scrotum before birth. In a typical pregnancy, the testicles develop in the abdomen and descend into the scrotum as the baby grows.
If this does not happen, the testicle remains in the abdomen or groin. This condition is most often detected in newborns and can affect about 3-5% of full-term infants and up to 30% of premature infants.
Side Effects of Cryptorchidism
If left untreated, cryptorchidism can lead to several potential complications:
- Fertility Issues: An undescended testicle may lead to lower sperm production or reduced fertility. The abnormal position of the testicle can affect sperm development due to the temperature being higher in the abdomen compared to the scrotum.
- Increased Risk of Testicular Cancer: Men with cryptorchidism have a higher risk of developing testicular cancer, especially if the condition is present in adulthood.
- Inguinal Hernia: There is an increased risk of inguinal hernia, where part of the intestine pushes through the abdominal wall or into the inguinal canal.
- Psychological Impact: Older children and adults may experience psychological effects related to the condition, including embarrassment or self-consciousness about their appearance or health.
How is Cryptorchidism Diagnosed?
Diagnosis of cryptorchidism typically involves a physical examination by a healthcare provider. In infants, this usually occurs shortly after birth. The doctor will assess the position of the testicles and may perform a thorough examination of the groin and abdomen.
If necessary, further imaging studies such as ultrasound or MRI may be used to locate the undescended testicle and determine its exact position.
Potential Treatment of Cryptorchidism
Treatment for cryptorchidism is important to prevent complications and is typically recommended if the testicle has not descended by the time the child is six months old. The primary treatment options include:
- Hormonal Therapy: Hormonal treatments, such as human chorionic gonadotropin (hCG) or luteinizing hormone-releasing hormone (LHRH), can sometimes stimulate the testicle to descend. This method is less commonly used but can be considered in specific cases.
- Surgical Intervention (Orchidopexy): The most common and effective treatment is surgical correction. This procedure, known as orchidopexy, involves moving the testicle into the scrotum and securing it in place. It is typically performed between the ages of 6 and 12 months. The surgery is minimally invasive and often done on an outpatient basis.
- Follow-up Care: After surgery, follow-up care is essential to ensure that the testicle remains in the correct position and to monitor for any potential complications.
👉 Contact us for further information and receive a complimentary consultation.

.webp)
 (1).webp)

.webp)
 (1).webp)


.webp)
 (1).webp)

.webp)
 (1).webp)
