What is Cystocele (Bladder Prolapse)?
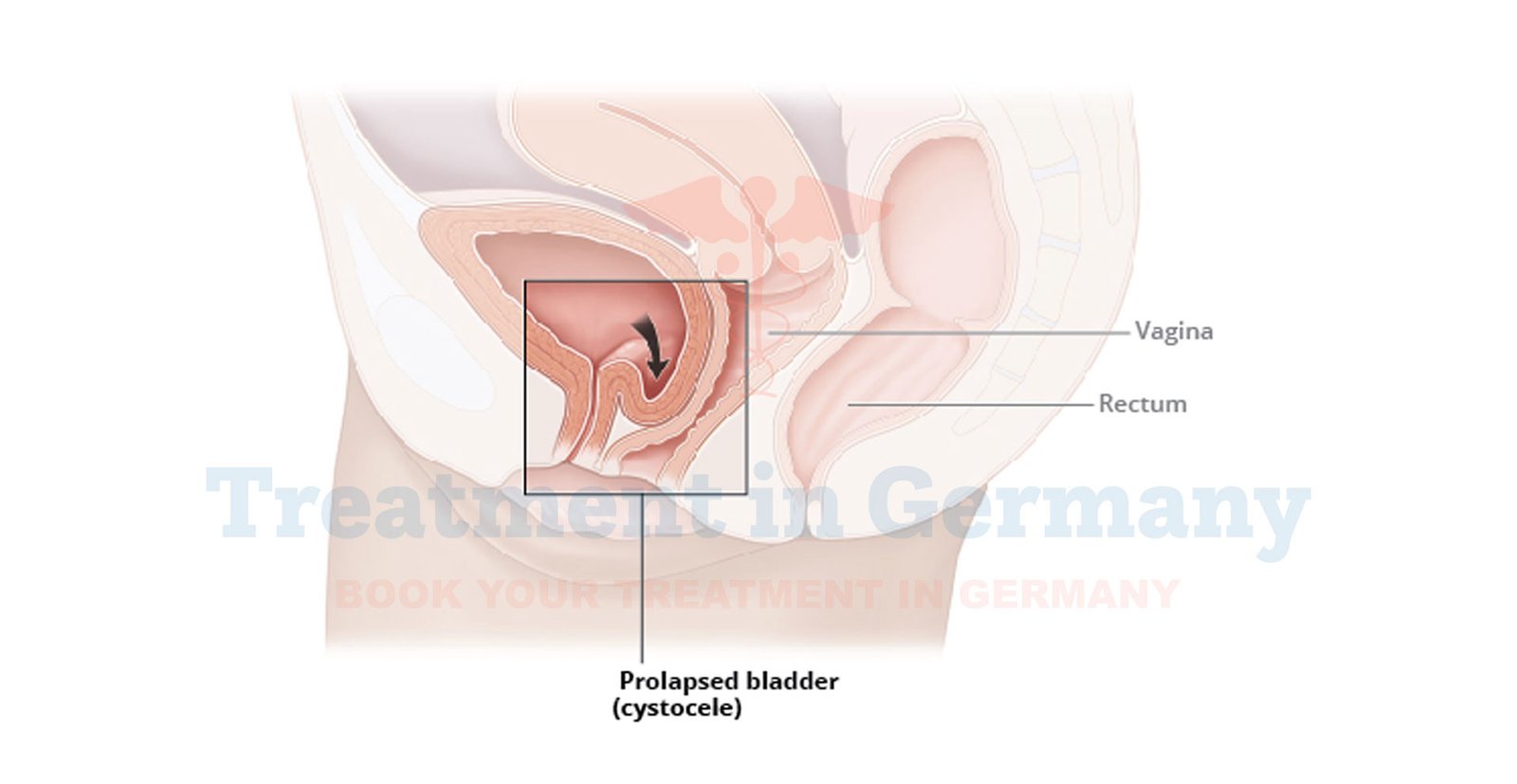
Cystocele, also known as bladder prolapse, occurs when the wall between a woman’s bladder and her vagina weakens and stretches, causing the bladder to bulge into the vaginal wall.
This condition is often associated with childbirth, aging, or heavy lifting, which can weaken the pelvic support structures. As a result, women may experience a noticeable bulge in the vaginal area and a range of urinary symptoms.
Side Effects of Cystocele (Bladder Prolapse)
The side effects and symptoms of cystocele can vary, but common issues include:
- Pelvic Pressure or Fullness: A feeling of heaviness or pressure in the pelvic region.
- Urinary Incontinence: Leakage of urine, particularly during activities that increase abdominal pressure such as coughing or sneezing.
- Frequent Urination: An increased need to urinate, often with a sense of urgency.
- Urinary Retention: Difficulty in fully emptying the bladder.
- Vaginal Bulge: A noticeable bulge or protrusion in the vaginal area, especially noticeable when standing or during physical activities.
- Discomfort During Intercourse: Pain or discomfort during sexual activity due to the prolapse.
How is Cystocele (Bladder Prolapse) Diagnosed?
Diagnosis of cystocele typically involves a combination of medical history, physical examination, and diagnostic tests:
- Medical History: Your doctor will inquire about your symptoms, any previous pregnancies, and other relevant health information.
- Physical Examination: A gynecological exam will be performed to assess the extent of the prolapse. The doctor may ask you to cough or perform a Valsalva maneuver to observe the prolapse's effect.
- Imaging Tests: In some cases, imaging studies like ultrasound or MRI may be used to get a detailed view of the prolapse and its severity.
- Urodynamic Testing: This involves measuring bladder function and can help assess the impact of the prolapse on urination.
Potential Treatment of Cystocele (Bladder Prolapse)
Treatment options for cystocele vary based on the severity of the condition and the symptoms experienced. In Germany, you can expect a comprehensive approach that may include:
- Lifestyle Changes: For mild cases, simple lifestyle modifications such as pelvic floor exercises (Kegel exercises), weight management, and avoiding heavy lifting can be effective in managing symptoms.
- Pessary Device: A pessary is a non-surgical device inserted into the vagina to support the bladder and prevent it from prolapsing further. It can be a temporary or long-term solution depending on your needs.
- Physical Therapy: Specialized pelvic floor physical therapy can strengthen the muscles supporting the bladder and improve symptoms.
- Surgical Options: For more severe cases, surgical intervention may be necessary. Procedures can involve repairing the weakened vaginal wall and repositioning the bladder. Common surgical options include anterior repair (also known as colporrhaphy) and the use of mesh to provide additional support.
👉 Contact us for further information and receive a complimentary consultation.

.webp)
 (1).webp)

.webp)
 (1).webp)


.webp)
 (1).webp)

.webp)
 (1).webp)
