What Are Esophageal Varices?
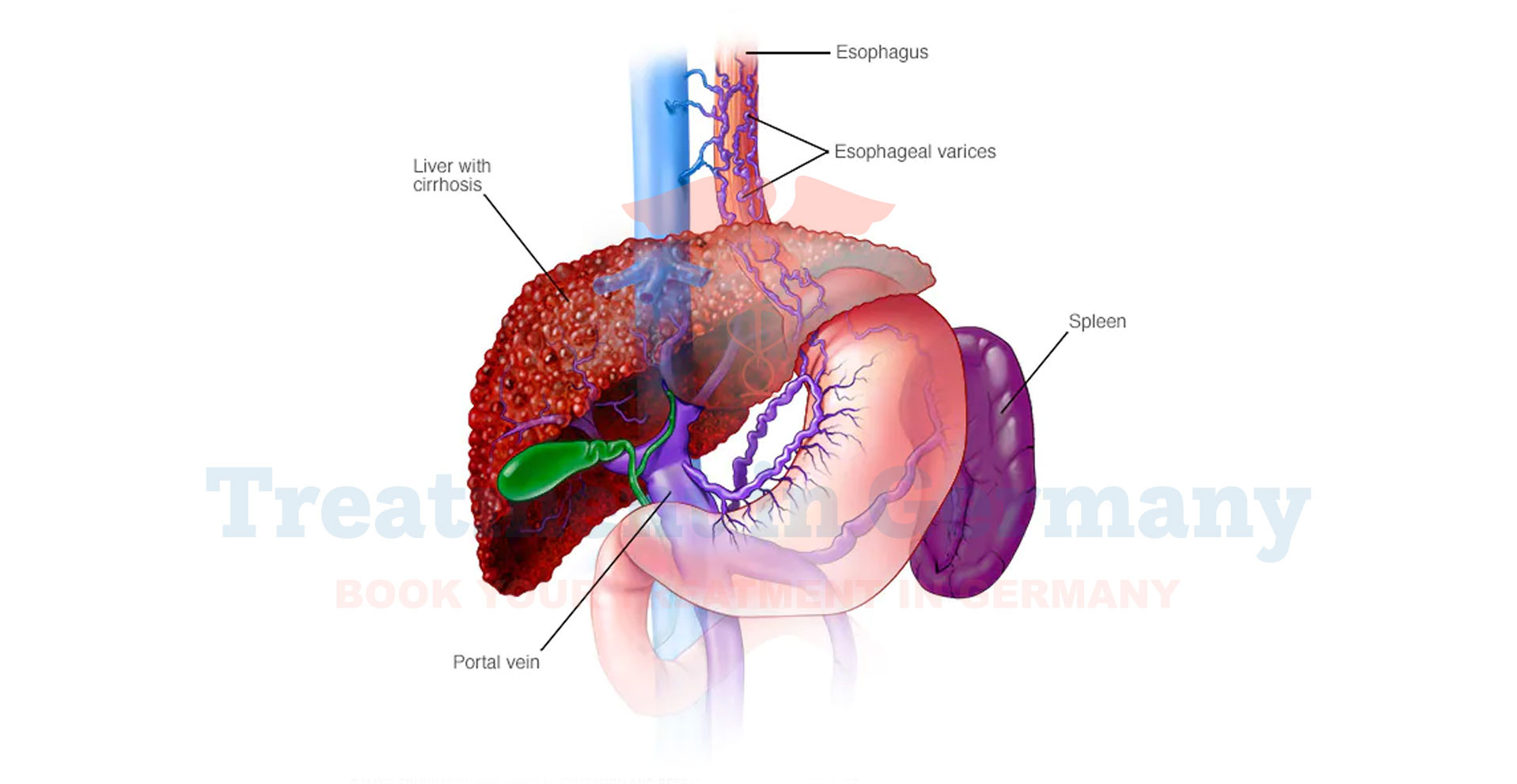
Esophageal varices are swollen veins located in the lower part of the esophagus, the tube that carries food from your mouth to your stomach.
These veins can become enlarged and fragile, typically as a result of increased pressure in the portal vein, which carries blood from the digestive organs to the liver.
This condition is often associated with severe liver diseases such as cirrhosis. When these varices rupture, they can lead to severe bleeding and other complications.
Side Effects of Esophageal Varices
The main concern with esophageal varices is the risk of bleeding. Symptoms of bleeding varices may include:
- Vomiting Blood: You may notice bright red blood or coffee-ground-like material in your vomit.
- Black or Tarry Stools: This indicates digested blood in your stool.
- Sudden Weakness or Dizziness: Caused by significant blood loss.
- Abdominal Pain: Particularly if the varices are inflamed or irritated.
If left untreated, the bleeding from esophageal varices can be life-threatening and requires immediate medical attention.
How Are Esophageal Varices Diagnosed?
Diagnosing esophageal varices typically involves a combination of tests and procedures:
- Endoscopy: An upper endoscopy, or esophagogastroduodenoscopy (EGD), is the primary method for diagnosing esophageal varices. During this procedure, a flexible tube with a camera is inserted through your mouth to visualize the esophagus and identify any varices.
- Imaging Tests: Ultrasounds, CT scans, or MRI can help assess the condition of the liver and blood flow, providing additional context for the presence of varices.
- Blood Tests: These tests can help evaluate liver function and detect any related issues that might be contributing to increased pressure in the portal vein.
Potential Treatment for Esophageal Varices
Treatment for esophageal varices focuses on managing and preventing complications, particularly bleeding. Common approaches include:
- Medications: Drugs such as beta-blockers may be prescribed to lower blood pressure in the portal vein and reduce the risk of variceal bleeding.
- Endoscopic Therapy: Band ligation or sclerotherapy is often used to treat varices. In band ligation, elastic bands are placed around the varices to cut off blood flow, causing them to shrink. Sclerotherapy involves injecting a solution to cause the varices to scar and close up.
- Shunt Procedures: In severe cases, a procedure called transjugular intrahepatic portosystemic shunt (TIPS) may be performed to create a new pathway for blood flow and reduce portal pressure.
- Liver Transplant: For patients with advanced liver disease, a liver transplant might be considered as a long-term solution to manage esophageal varices and underlying liver issues.
👉 Contact us for further information and receive a complimentary consultation.

.webp)
 (1).webp)

.webp)
 (1).webp)


.webp)
 (1).webp)

.webp)
 (1).webp)
