What is Genitourinary Prolapse?
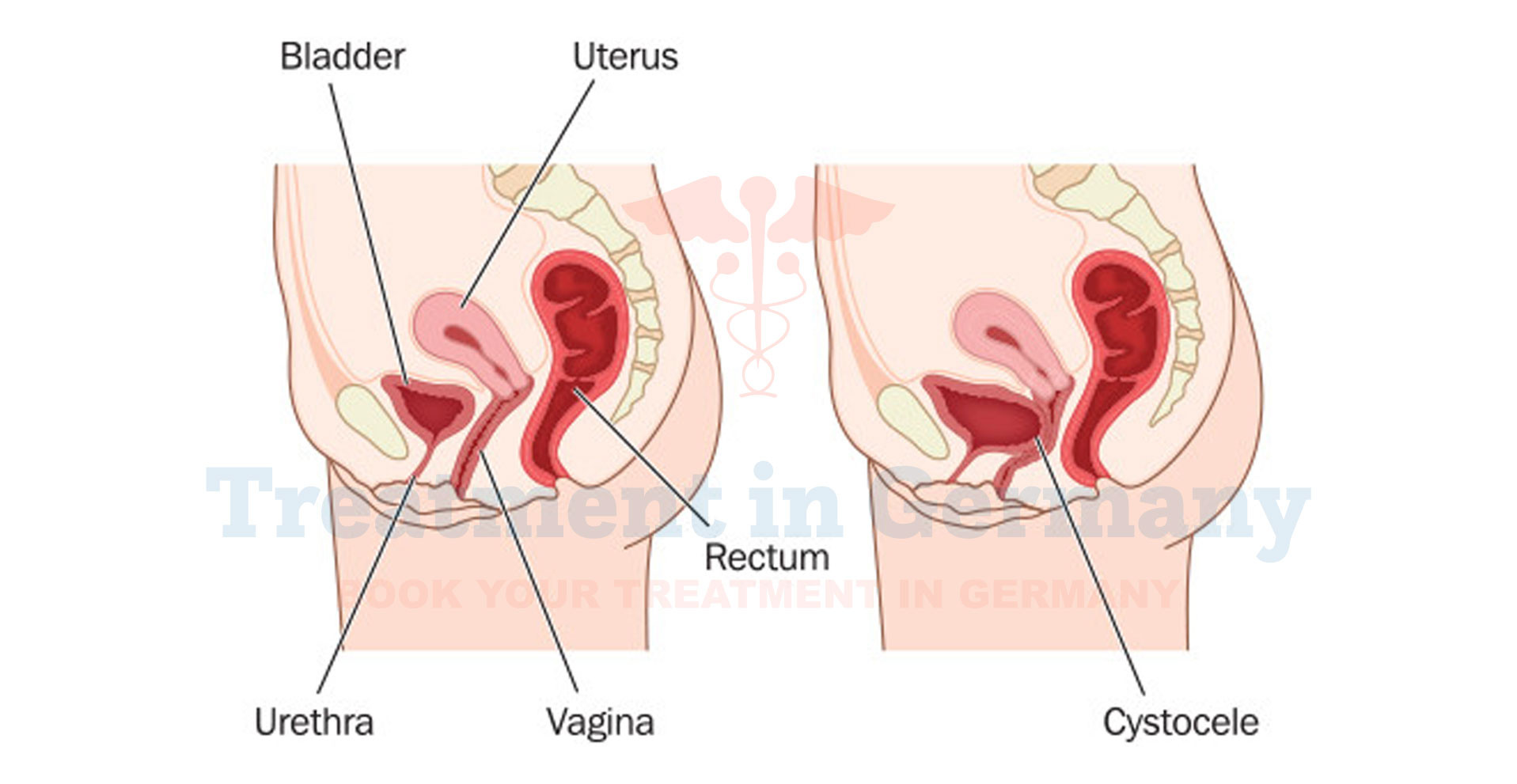
Genitourinary prolapse occurs when the structures of the pelvic floor weaken, causing organs like the bladder, uterus, or rectum to bulge into the vaginal wall.
This condition can lead to discomfort and a range of symptoms affecting daily life. In women, this often involves a prolapse of the bladder (cystocele), uterus, or rectum (rectocele), whereas men might experience a prolapse of the bladder or rectum.
This condition is commonly associated with childbirth, aging, or chronic conditions that put pressure on the pelvic floor.
Side Effects of Genitourinary Prolapse
The side effects and symptoms of genitourinary prolapse can vary depending on the severity and type of prolapse. Common issues include:
- Pelvic Pressure: A feeling of heaviness or pressure in the pelvic region.
- Urinary Symptoms: Frequent urination, urinary incontinence, or difficulty emptying the bladder.
- Bowel Problems: Difficulty with bowel movements or a sensation of incomplete evacuation.
- Pain: Discomfort or pain during intercourse.
- Visible Bulge: In more severe cases, a noticeable bulge may be visible through the vaginal opening.
How is Genitourinary Prolapse Diagnosed?
Diagnosing genitourinary prolapse involves a combination of medical history, physical examination, and sometimes imaging studies. The diagnostic process typically includes:
- Medical History: Discussing symptoms, medical history, and any factors that might contribute to pelvic floor weakness.
- Physical Examination: A gynecological or urological examination to assess the pelvic floor and identify any signs of prolapse.
- Imaging Studies: In some cases, ultrasound or MRI may be used to evaluate the extent of the prolapse and any associated issues.
Potential Treatment of Genitourinary Prolapse
Treatment for genitourinary prolapse depends on the severity of the condition and its impact on your quality of life. Options include:
- Lifestyle Changes: Weight management, pelvic floor exercises (such as Kegels), and managing chronic cough or constipation can help alleviate symptoms and prevent progression.
- Physical Therapy: Specialized pelvic floor physical therapy can strengthen the muscles and support structures of the pelvic area.
- Pessary: A pessary is a device inserted into the vagina to support the prolapsed organs and alleviate symptoms.
- Surgical Options: In cases where conservative measures are insufficient, surgical intervention may be necessary. Various surgical techniques can repair the prolapse and support the pelvic organs.
👉 Contact us for further information and receive a complimentary consultation.

.webp)
 (1).webp)

.webp)
 (1).webp)


.webp)
 (1).webp)

.webp)
 (1).webp)
