What is Neurogenic Bladder?
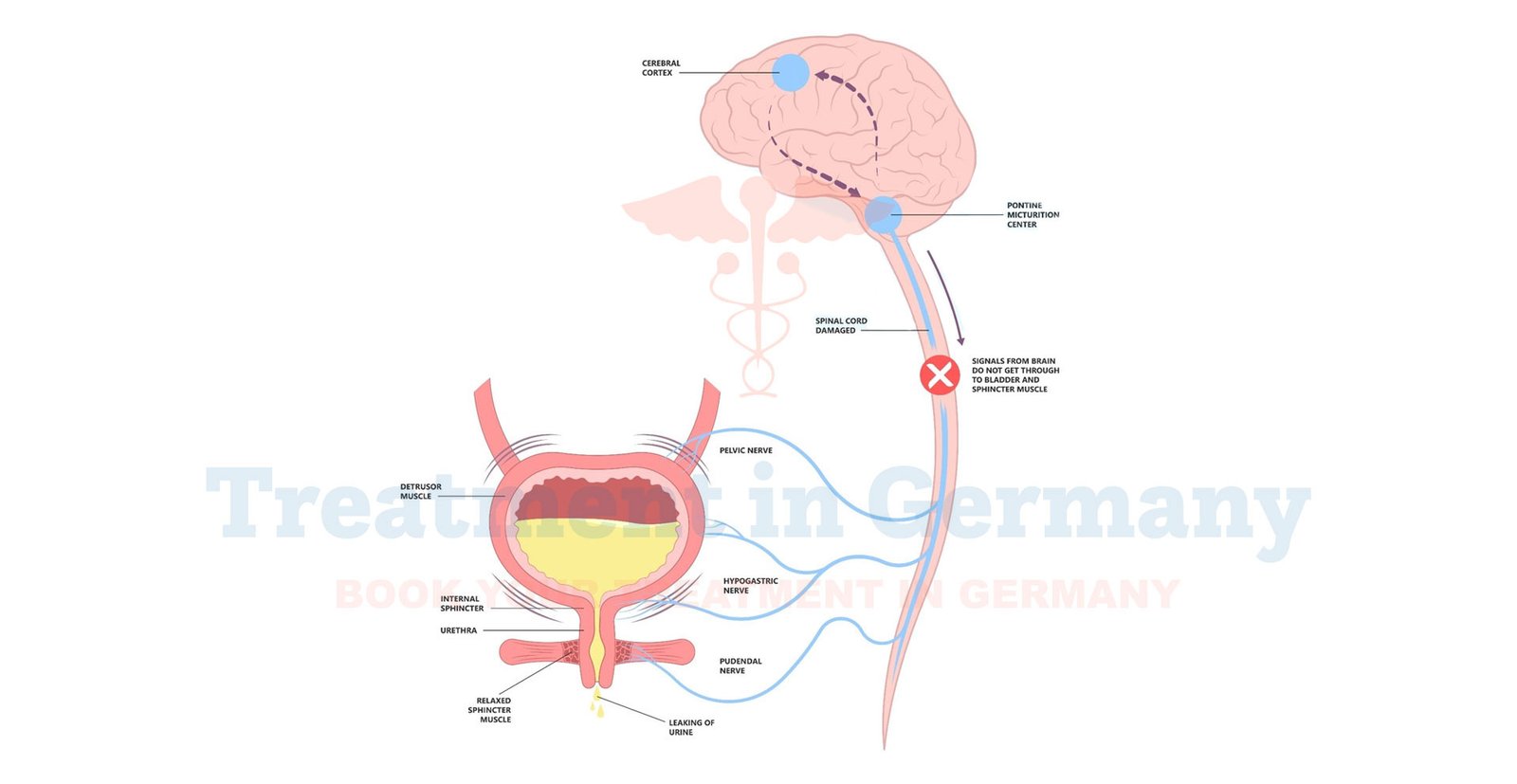
Neurogenic bladder is a condition where nerve damage impairs the bladder’s ability to store and/or release urine properly.
This damage can stem from various neurological conditions such as spinal cord injuries, multiple sclerosis, or stroke. As a result, the bladder may become overactive or underactive, leading to difficulties with urination, frequent infections, and other related issues.
Side Effects of Neurogenic Bladder
Neurogenic bladder can manifest in several ways, each affecting daily life and overall health. Common side effects include:
- Frequent Urination: The need to urinate more often than usual.
- Urgency: A sudden, strong urge to urinate.
- Incontinence: Uncontrolled leakage of urine.
- Urinary Retention: Difficulty fully emptying the bladder, leading to discomfort and potential infections.
- Recurrent Urinary Tract Infections (UTIs): Increased risk of infections due to incomplete bladder emptying or catheter use.
- Kidney Damage: Prolonged issues can impact kidney function, potentially leading to more severe health problems.
How is Neurogenic Bladder Diagnosed?
Diagnosis of neurogenic bladder typically involves a comprehensive approach:
- Medical History and Physical Examination: A detailed review of symptoms and medical history, along with a physical exam, helps identify possible causes.
- Neurological Examination: To assess nerve function and identify any neurological conditions affecting the bladder.
- Urodynamic Testing: This series of tests measures bladder pressure and function to evaluate how well the bladder is storing and releasing urine.
- Imaging Studies: Ultrasound, MRI, or CT scans may be used to visualize the bladder and surrounding structures.
- Urinalysis: Testing urine samples for infections or abnormalities.
Potential Treatment of Neurogenic Bladder
Treatment options for neurogenic bladder in Germany are tailored to individual needs and the underlying cause of the condition. Common approaches include:
- Medications: Drugs to manage symptoms such as bladder spasms, infections, or incontinence.
- Catheterization: Intermittent or continuous catheterization helps manage bladder emptying and reduce the risk of infections.
- Bladder Training: Techniques to retrain the bladder to function more effectively, such as scheduled voiding or pelvic floor exercises.
- Neuromodulation Therapy: Electrical stimulation of nerves to improve bladder function.
- Surgical Interventions: In severe cases, surgical options such as bladder augmentation or artificial sphincters may be considered.
- Lifestyle and Dietary Adjustments: Modifications to diet and fluid intake can also help manage symptoms.
👉 Contact us for further information and receive a complimentary consultation.

.webp)
 (1).webp)

.webp)
 (1).webp)


.webp)
 (1).webp)

.webp)
 (1).webp)
