What is Patellar Tendinitis (Jumper's Knee)?
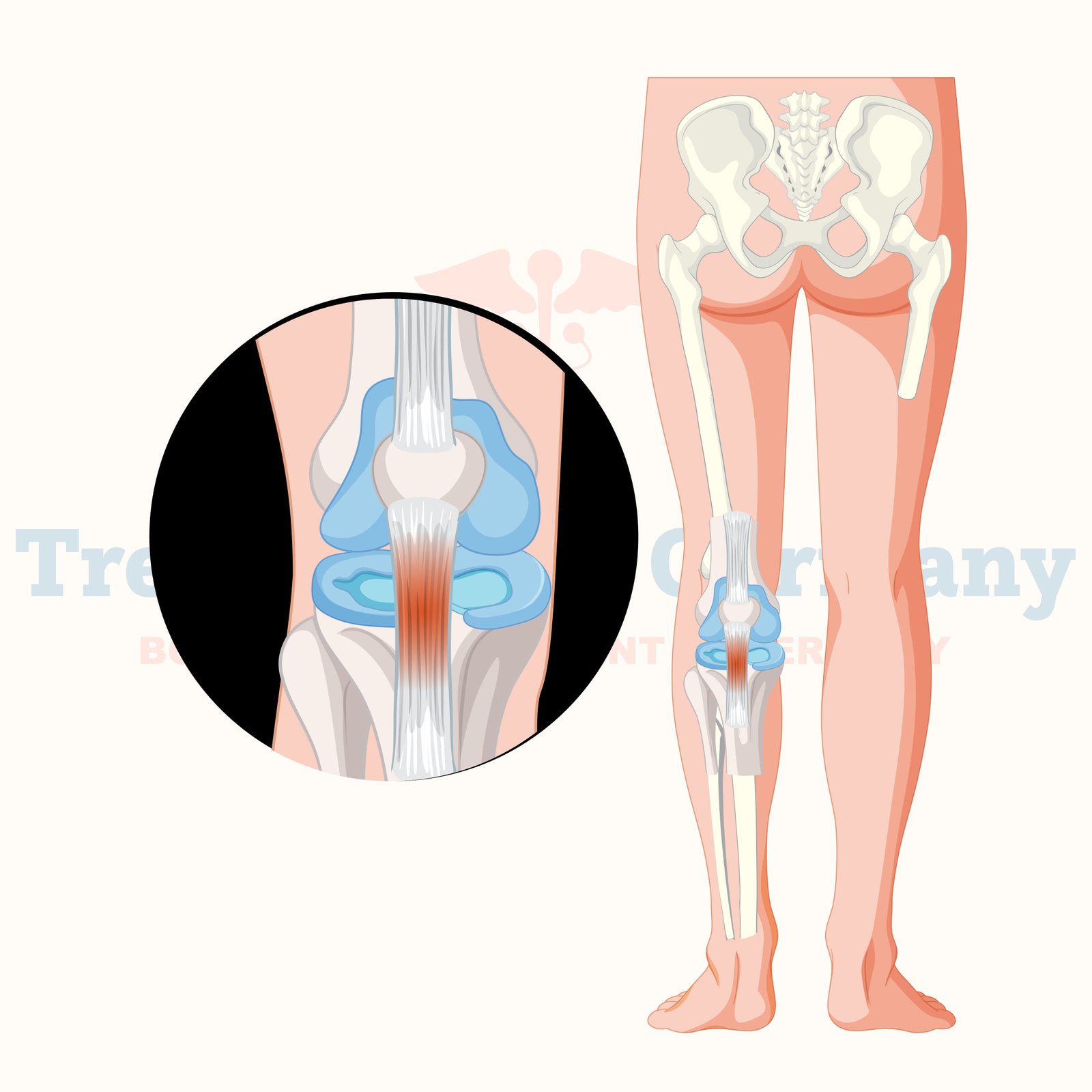
Patellar tendinitis, also known as Jumper's Knee, is an overuse injury affecting the patellar tendon, which connects the kneecap (patella) to the shinbone (tibia).
This condition is common among athletes who frequently jump, such as basketball and volleyball players, but it can also affect individuals who engage in repetitive knee-stressing activities.
Patellar tendinitis is characterized by inflammation, micro-tears, and degeneration of the tendon, leading to pain and impaired knee function.
Patellar tendinitis, also referred to as "jumper's knee," is an overuse injury involving the tendon that joins the kneecap (patella) to the shinbone (tibia). This tendon, known as the patellar tendon, is essential for knee extension, allowing people to jump, run, and carry out other knee movement activities.
Jumper's knee is most common among athletes participating in sports that require regular jumping, such as basketball, volleyball, and track & field. However, it may also affect non-athletes who engage in frequent knee-bending exercises.
What is Patellar Tendinitis?
Patellar tendinitis is inflammation, irritation, and tiny tears in the patellar tendon. The problem often develops gradually due to frequent stress on the knee joint, causing knee pain and discomfort right below the kneecap. If left untreated, patellar tendinitis may progress over time, causing constant pain and impaired knee function.
Jumper's knee is persistent among athletes who engage in sports injury that require high-impact motions. However, it may also affect those with occupations or hobbies requiring frequent kneeling or bending. While jumping sports are often connected with the injury, it may happen to anybody who puts too much pressure on their knee tendons.
Causes of Patellar Tendinitis
Patellar tendinitis is most often caused by repeated tension and overuse of the patellar tendon. This causes microscopic rips in the tendon fibers, resulting in inflammation and weakening over time—a variety of reasons, including may cause patellar tendinitis.
- Repetitive leaping and running: Athletes who participate in sports requiring frequent running jumping, sprinting, and abrupt pauses are more likely to develop patellar tendinitis. The continual tension on the knee tendon might result in overuse problems.
- Poor biomechanics: Improper leg muscles, foot, or hip posture during physical exercise may put additional pressure on the patellar tendon. Flat feet, tight muscles, and weak Quadriceps may all contribute to biomechanical problems that raise the likelihood of patellar tendinitis.
- Inadequate warm-up and stretching: Failure to properly warm up and stretch before activity may cause tightness in the quadriceps and hamstrings, putting additional strain on the patellar tendon.
- Sudden increase in activity: Beginning a new sport or training program may overload the patellar tendon and develop tendinitis.
- Improper footwear: Wearing shoes with insufficient support or cushioning might lead to patellar tendonitis feel by affecting how stresses are transmitted across the knee joint.
Symptoms of patellar tendinitis
Patellar tendinitis symptoms usually develop gradually and might worsen if left untreated. Common symptoms include:
- Pain and tenderness below the kneecap: Pain is often felt right under the kneecap, where the patellar tendon connects to the tibia. This discomfort may initially be moderate and only occur after physical exercise, but it may worsen and remain as the condition progresses.
- Swelling and inflammation: Tendon irritation may cause the affected region to become swollen, warm to the touch, and inflamed.
- Knee stiffness: People with patellar tendinitis often report knee stiffness, particularly after inactivity or in the morning.
- Pain during physical activities: Jumping, jogging, bending, or kneeling may cause additional pain. In severe situations, walking or ascending stairs might be uncomfortable.
- Reduced range of motion: Patellar tendinitis may cause the knee joint to lose flexibility and range of motion over time.
Diagnosis of patellar tendinitis
Patellar tendinitis is diagnosed by a combination of medical history, physical examination, and imaging tests.
- Medical history: The healthcare professional will inquire about the patient's symptoms, activity level, and any recent changes in fitness routine or training habits. They'll also ask about any past knee injuries.
- Physical examination: The doctor will check the knee for soreness, edema, and range of motion. The doctor may also use particular tests to assess quadriceps strength and hamstring flexibility.
Imaging tests:
- X-rays: Although they cannot see soft tissue injuries like tendinitis, they may rule out other possible reasons for knee discomfort, such as fractures or bone spurs.
- Ultrasound: This imaging tool visualizes the patellar tendon in real-time, enabling doctors to identify inflammation, thickness, or tears.
- Magnetic Resonance Imaging (MRI): An MRI may give comprehensive pictures of the patellar tendon and adjacent structures, assisting in determining the severity of the injury and any related soft tissue damage.
Treatment for Patellar Tendinitis
The therapy of patellar tendinitis is determined by the degree of the injury and the patient's level of activity. Options vary from conservative care to more complex procedures in extreme situations.
Nonsurgical Treatment
Rest and activity modification: The first step in treating patellar tendinitis is to limit or eliminate activities that exacerbate the symptoms. Rest enables the tendon to repair and avoids further injury. Athletes may need to suspend or change their training schedules to avoid straining the knee.
- Ice therapy: Applying ice to the affected area for 15-20 minutes many times daily may help decrease pain and inflammation.
- Physical therapy: An organized physical therapy program is necessary to improve strength, flexibility, and tendon repair. Physical therapists lead patients through exercises that target the quadriceps, hamstrings, and calf muscles to reduce stress on the patellar tendon and improve knee function.
- Nonsteroidal anti-inflammatory medicines (NSAIDs): Over-the-counter pain Treatment in germany.such as ibuprofen or naproxen can assist with relieving discomfort and inflammation in the early stages of patellar tendinitis.
- Patellar tendon strap: A patellar tendon strap, also known as a knee brace or jumper's knee strap, may be used when exercising to distribute pressure over the tendon and ease discomfort.
Advanced Treatment Options.
More advanced techniques may be sought when conservative therapies do not give enough relief.
- Corticosteroid injections: In certain circumstances, corticosteroid injections may be given directly into the patellar tendon to decrease inflammation and offer comfort. However, these injections should be used with caution, since regular use may weaken the tendon and increase the reduce your risk of tearing.
- Platelet-rich plasma (PRP) treatment: In PRP therapy, concentrated platelets from the patient's blood are injected into the patellar tendon to stimulate healing and tissue regeneration. This therapy is often used for chronic or severe patellar tendonitis.
- Extracorporeal shockwave treatment (ESWT): High-energy sound waves encourage repair in the patellar tendon by increasing blood flow and decreasing discomfort. This non-invasive therapy is becoming more popular for tendon injuries that do not respond to conventional.
- Surgical intervention: In certain situations, surgery may be required to remove damaged tissue and restore the patellar tendon. sports medicine and arthroscopic surgery is usually reserved for those with severe, long-standing patellar tendonitis who have not responded to previous therapies.
Recovery and Rehabilitation.
Patellar tendinitis recovery duration varies depending on the severity of the injury and how well the person follows the treatment plan. Mild instances may improve after a few weeks of rest and physical treatment; however, more severe cases might take several months to completely recover.
Rehabilitation is progressively reintroducing physical activity while limiting stress on the patellar tendon. Physical therapists are essential in assisting patients through rehabilitation, ensuring they regain strength, flexibility, and good biomechanics.
Return to sports or physical activities cautiously and gradually increase intensity to prevent re-injury. Patellar tendinitis may develop chronically if not treated appropriately; long-term preventative methods are required.
Prevention of patellar tendinitis
To prevent patellar tendinitis, address the underlying risk factors and adopt healthy practices that limit tension on the patellar tendon. Here are some preventative measures:
- Proper warm-up and stretching: Always warm up before participating in physical activity, and include dynamic stretches for the quadriceps, hamstrings, and calf muscles.
- Strengthening exercises: Work on strengthening the muscles around the knee, such as the quadriceps, hamstrings, and calves, to enhance stability and lower the chance of tendon problems.
- Wear appropriate footwear: Wear shoes that offer suitable support and cushioning for your feet and knees, particularly while participating in high-impact activities.
- Avoid sudden increases in activity: Exercise for longer periods and at a higher intensity gradually to give your body time to adapt and get stronger.
- Cross-training: Include low-impact sports, such as swimming or cycling, in your workout plan to avoid repeated stress on the patellar tendon.
👉 Contact us for further information and receive a complimentary consultation.

.webp)
 (1).webp)

.webp)
 (1).webp)


.webp)
 (1).webp)

.webp)
 (1).webp)
