The Department of Radiation Oncology plays an important role in cancer treatment by using targeted radiation therapy to kill cancer cells and reduce tumors. This specialized medical field integrates advanced technology and therapeutic techniques to manage and treat various types of cancer, offering hope for patients through effective and often life-saving interventions.
2) Treatment Planning:
Simulation: A process where imaging studies are used to create a detailed map of the tumor and surrounding tissues. This helps in accurately targeting the radiation beams and planning the treatment.
Dosimetry: The calculation of the appropriate dose of radiation required to effectively treat the tumor while minimizing exposure to healthy tissues. Dosimetrists work closely with radiation oncologists to ensure precise dosing.
3) Technology and Equipment:
Linear Accelerators: (Linacs): Machines that generate high-energy radiation beams for external beam radiation therapy. Linacs are equipped with advanced imaging systems to guide treatment delivery.
CT Scanners: Used for imaging and treatment planning. CT scans provide detailed cross-sectional images of the body, allowing for accurate localization of tumors.
MRI Scanners: Provide high-resolution images of soft tissues and are used with CT scans for detailed treatment planning.
PET Scanners: Changes in metabolic activity may help measure tumor response to therapy.
4) Multidisciplinary Care:
Oncologists: Radiation oncologists specialize in using radiation therapy to treat cancer and work closely with other healthcare professionals to develop personalized Treatment in germany plans.
Medical Physicists: Ensure the safe and accurate delivery of radiation therapy by calibrating equipment and verifying treatment plans.
Dosimetrists: Calculate the precise radiation doses required for each patient and design treatment plans based on clinical guidelines.
Radiation Therapists: Operate the radiation equipment and give treatments by the specified plan.
Nurses and Support Staff: Provide patient care, education, and emotional support throughout the treatment process.
Diagnostic Approaches
Accurate diagnosis and treatment planning are critical for effective radiation therapy. The diagnostic process involves several steps:
1) Initial Consultation:
Medical History: Review of the patient’s medical history, including previous treatments, health conditions, and current symptoms.
Physical Examination: Evaluation of the patient’s overall health and specific areas of concern.
2) Imaging Studies:
CT Scans: Detailed imaging of the body to identify and map the tumor and surrounding structures.
MRI Scans: High-resolution images of soft tissues to provide additional information about the tumor and its relationship to nearby structures.
PET Scans: Assess the metabolic activity of tumors and evaluate their response to treatment.
3) Biopsy:
Tissue Sample: A small sample of tissue is taken from the tumor to confirm the diagnosis and determine the type and grade of cancer.
4) Treatment Simulation:
Positioning and Marking: The patient is positioned on a treatment table, and markers or immobilization devices are used to ensure consistent positioning for each treatment session.
Treatment Planning: Advanced imaging and computer software are used to develop a precise treatment plan, including the angle and intensity of radiation beams.
Treatment Strategies
The Department of Radiation Oncology utilizes various treatment strategies to manage and treat cancer effectively:
1) External Beam Radiation Therapy (EBRT):
3D Conformal Radiation Therapy (3DCRT): Delivers radiation from multiple angles to precisely target the tumor while minimizing exposure to healthy tissues.
Intensity-Modulated Radiation Therapy (IMRT): Uses advanced technology to modulate the intensity of radiation beams, allowing for more precise targeting of tumors and better sparing of surrounding healthy tissues.
Stereotactic Radiosurgery (SRS): A highly precise form of radiation therapy that delivers a high dose of radiation to a small, well-defined tumor in a single session or a few sessions. It is often used for brain tumors and other localized cancers.
2) Internal Radiation Therapy (Brachytherapy):
Prostate Brachytherapy: Involves placing radioactive seeds directly into the prostate gland to treat prostate cancer.
Breast Brachytherapy: Involves placing a radioactive source inside or near the breast tumor to target cancer cells while preserving healthy tissue.
Cervical Brachytherapy: Involves inserting a radioactive source into the cervical canal to treat cervical cancer.
3) Systemic Radiation Therapy:
Radioactive Iodine Therapy: Used to treat thyroid cancer by administering radioactive iodine that specifically targets thyroid cells.
Radionuclide Therapy: Involves using radioactive substances to target cancer cells throughout the body, such as in the treatment of metastatic prostate cancer.
4) Combination Therapies:
Radiation and Chemotherapy: Combining radiation therapy with chemotherapy to enhance treatment effectiveness and target cancer cells from multiple angles.
Radiation and Surgery: Using radiation therapy before or after surgery to shrink tumors or eliminate residual cancer cells.
Side Effects and Management
While radiation therapy is an effective cancer treatment, it can cause side effects that vary depending on the treatment area and dosage:
1) Common Side Effects:
Fatigue: A common side effect that may persist for several weeks after treatment.
Skin Irritation: Pain, redness, or dryness where the treatment was applied.
Hair Loss: Temporary hair loss in the treatment area.
Nausea and Vomiting: Particularly if the treatment area includes the abdomen or pelvis.
2) Management and Support:
Symptom Management: Medications and supportive care to alleviate side effects such as nausea, pain, and skin irritation.
Nutritional Support: Dietary counseling to maintain a healthy diet and manage side effects related to appetite and digestion.
Psychological Support: Counseling and support groups to help patients cope with the emotional challenges of cancer treatment.
Advances and Research in Radiation Oncology
The field of radiation oncology is continually evolving with new technologies and research improving treatment options and outcomes:
1) Precision Radiation Therapy:
Adaptive Radiation Therapy: Adjusts treatment plans based on changes in tumor size or patient anatomy during treatment.
Image-guided Radiation Therapy (IGRT): Uses advanced imaging techniques to ensure precise targeting of tumors and minimize radiation exposure to healthy tissues.
2) Proton Therapy:
Proton Beam Therapy: Uses protons instead of X-rays to deliver radiation to tumors, offering the potential for more precise targeting and reduced side effects.
3) Radiogenomics:
Personalized Treatment: The study of genetic factors that influence how tumors respond to radiation therapy, enabling more tailored and effective treatment plans.
4) Combination Therapies:
Immunoradiotherapy: Combines radiation therapy with immunotherapy to enhance the body’s immune response against cancer cells.
5) Clinical Trials:
Research Studies: Ongoing clinical trials test new radiation therapy techniques, drugs, and combination treatments to improve efficacy and reduce side effects.
Patient Education and Support
Educating patients and their families is essential for effective radiation therapy and recovery. The department provides various resources and support services:
Counseling Services: Offer emotional and psychological support to help patients cope with the stress and challenges of cancer treatment.
Support Groups: Facilitate connections between patients who have similar experiences, offering mutual support and sharing resources.
Educational Resources: Include brochures, websites, and seminars to provide information about radiation therapy, treatment options, and self-care strategies.
Patient Navigators: Assist patients in navigating the healthcare system, coordinating care, and addressing any concerns or barriers to treatment.
Radiation therapy employs high-energy radiation to kill cancer cells and shrink tumors. Radiation damages cancer cells' DNA, preventing them from growing and multiplying. Healthy cells are less damaged because they are more capable of healing.
Radiation therapy is typically safe and effective, although it might have adverse effects that differ based on the treatment location and dose. Most side effects are transient and may be handled with supportive care. Radiation therapy's advantages in cancer treatment often exceed its hazards.
The length of radiation therapy varies according to the kind and location of the cancer, as well as the treatment regimen. A normal regimen might run from a few weeks to several months and include daily or weekly treatments.
During a radiation therapy session, you will recline on a treatment table while the radiation equipment is set up to administer precise dosages of radiation. The process is normally painless and takes a few minutes. You may need to stay motionless to ensure proper treatment.
Managing side effects requires a combination of medications, dietary changes, and supportive interventions. Your healthcare provider will help you manage particular side effects such as skin irritation, exhaustion, and nausea. Regular follow-up sessions will assist to monitor and resolve any concerns that occur.
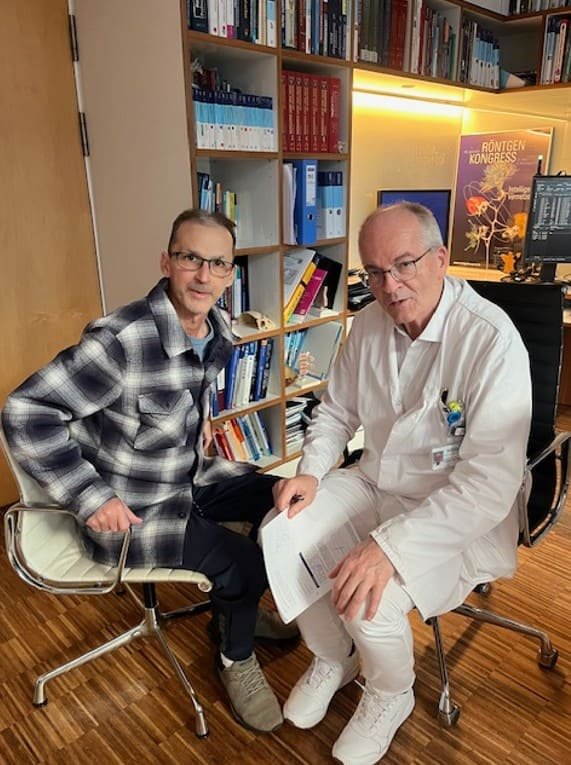
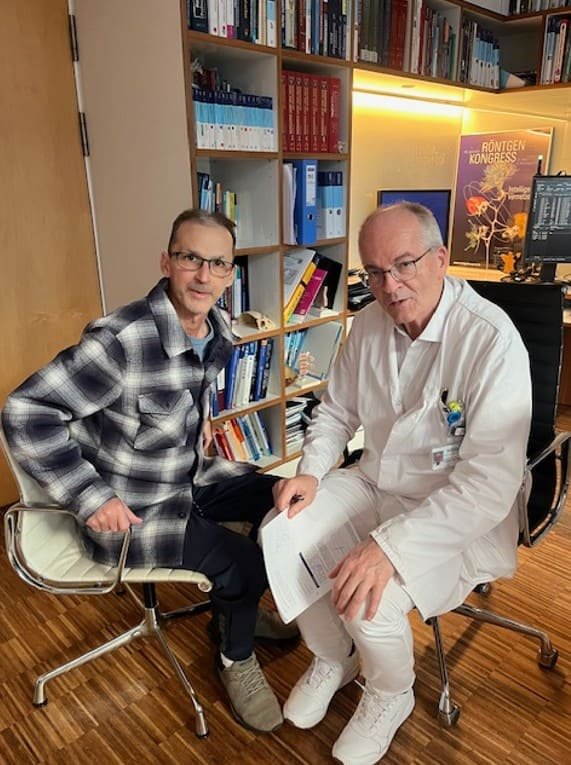
Experience the difference that expertise and compassion can make. Meet our exceptional team of experienced doctors, and trust us to provide you with the best in healthcare.

Radiation Oncology
Chief physician in radiotherapy and radiation oncology
Berlin


Radiation Oncology
Director of the Clinic for Radiooncology and Radiation Therapy.
Berlin

.webp)
 (1).webp)
.webp)
 (1).webp)


.webp)
 (1).webp)
.webp)
 (1).webp)
